Date of Publication.
Germany, 5. 2015
Authors
Manolakis K. DDS, Tsifoutakos D. MDT, Nikolaou G. MDT
Journal
Implantologie Journal 5 | 2015, Oemus Publishing Group
INDEX
Due to the demographic change in most highly developed industrial countries, implant prosthetic care of older patients is increasingly becoming the focus of professional interest. The following case report of a 73-year-old patient shows that the associated developments in implantology enable predictable restorations on just a few implants without extensive pre-treatment measures.
The present case report shows that the treatment with six implants and a conditionally removable CAD/CAM-manufactured bridge made of zirconium dioxide ceramic leads to a functionally and esthetically pleasing clinical outcome. Transfer of the functional and morphological parameters from the interim restoration to the design of the definitive reconstruction led to a predictable clinical result and to a high level of patient satisfaction.
Upper jaw total reconstruction utilizing root-shaped implants and a cross-arch monolithic zirconia bridge – case presentation.
Due to the demographic change in most highly developed industrial countries, implant prosthetic care of elderly patients is increasingly becoming the focus of professional interest. The following case report of a 73-year-old patient shows that the associated further developments in implantology enable predictable restorations on a reduced number of implants without extensive pretreatment measures.
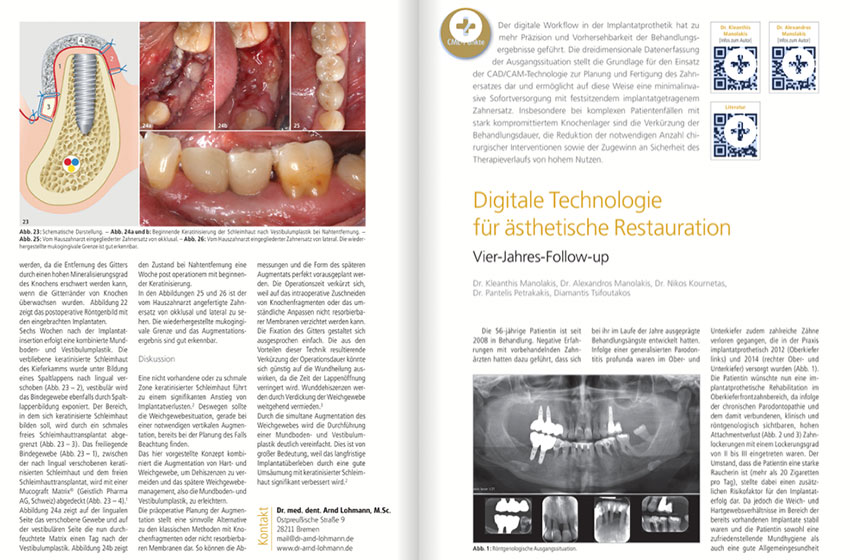
Introduction: The female patient presented in the following report came to our practice expressing the desire for a fixed restoration in the upper jaw. She had been fitted with a mucosa-supported partial prosthesis for twelve years. The existing prosthesis was retained to the last remaining tooth #27 by metallic clasps. She was also wearing a removable partial denture in the lower jaw, which was attached to the three remaining teeth #33, #32 and #43 by means of clasps.
Diagnosis: Anchor tooth 27 was condemned due to loss of periodontal supportive tissue and high degree of mobility. Although teeth in the upper jaw had been lost due to periodontal disease, sufficient bone was found radiologically. A digital volume tomography (CBCT) confirmed the panoramic X-ray findings.
Treatment planning: After thorough examination it was decided on a treatment plan involving a total of six implants and a conditionally removable screw-retained prosthetic reconstruction made of zirconium dioxide ceramic. Due to the adequately dimensioned crestal bone available no complex augmentation measures were necessary. Based on the “All-on-Six” concept (Pomares 2010) insertion of six root-shaped implants was planned (BEGO Semados® RSX, BEGO Implant Systems GmbH & Co. KG, Germany). Deviating from the treatment concept mentioned above, implant insertion was not planned transgingivally, but with the formation of a mucoperiosteal flap in order to ensure visual control of the surgical field. Furthermore, implants should not be loaded immediately, but only after a two-month submerged healing period. The transitional prosthetic restoration after implant uncovering should be carried out with a screw-retained provisional bridge. Definitive restoration should be inserted after the interim bridge has been in use for three to six months; a screw retained conditionally removable cross-arch bridge made of zirconium dioxide on Sub-Tec MultiPlus abutments (BEGO Implant Systems GmbH & Co. KG, Germany).
Surgical implant placement: After mucoperiosteal flap reflection a total of six titanium implants were inserted in one session under local anesthesia in areas #14, #12, #11, #22, #23, #25. In area #14 a 15 x 4.5 mm implant was placed. 4.1 x 13 mm implants were inserted in areas #12, #23 and #25; finally, in the incisor areas #11 and #22 two implants with the same length but with a 3.75mm diameter were placed. The relatively good bone availability present meant that the two terminal implants in regions 14 and 25 should not be angled, as in the majority of patient cases, but could be inserted parallel to the adjacent implants. Cover screws were placed and mucoperiosteal flaps were re-adapted without tension using individual sutures. Postoperatively taken panoramic image showed proper implant positioning. Although parallel pins were used, optimal axial alignment could not be achieved with all implants. Prosthetic compensation of slight implant divergences could be made possible in an elegant way by means of the system-specific multiunit abutments in the laboratory. Tooth #27 was initially preserved during the two-month implant healing phase to stabilize the partial denture. Existing prosthesis was relined and served as a temporary solution until implant uncovering.
Treatment: an impression for the interim bridge fabrication was taken at two-month healing period in an open tray procedure using an individual impression tray. Color-coded impression posts were used for the different implant diameters. The A-silicone Variotime Putty/Variotime Light Flow (Heraeus Kulzer GmbH, Hanau, Germany) was used. Variotime is characterized by short setting times in the mouth, high final hardness and very good dimensional stability. A master model was then fabricated in the laboratory based on the impression. After the gingival mask had been applied, MultiPlus abutments and corresponding plastic cylinders were inserted. In the case of implant restoration in the anterior region palatal positioning of the fastening screws is an important treatment objective for aesthetic reasons. The MultiPlus system offers angled abutments for this purpose. Four 20 degrees angled abutments were used on the four anterior implants, while straight abutments could be used on the two distal implants. Burn out Polyoxymethylene (POM) wax sleeves were used as connecting elements for the wax modeling of the metal framework. Prefabricated plastic veneers (artVeneer, Merz Dental GmbH, Germany), which are characterized by optimal esthetic and mechanical properties, served as veneering material for the interim prosthesis.
Before interim bridge insertion abutments were screwed onto the implants with a torque of 30 Ncm. The temporary bridge was then screwed onto the abutments according to the manufacturer’s instructions with 20 Ncm. Final functional and esthetic control showed satisfactory clinical results. In the following wearing period of four months hard and soft tissue was able to consolidate in the surgical area. Definitive prosthetic restoration was carried out with a zirconium dioxide bridge made using CAD/CAM, fabricated from a polychrome high-performance zirconium dioxide blank (Katana Zirconia Multi Layered ML, Kuraray Noritake Dental Inc). In a special manufacturing layering process these blanks are layered with enamel and dentine shades. This fact results in a natural color gradient, already achieved with the zirconium dioxide framework.
The CAD/CAM manufactured bridge framework was fabricated using the dentCare software (REITEL Feinwerktechnik GmbH, Bad Essen, Germany). An individualization of the vestibular surfaces of the reconstruction was achieved by staining ceramics. Several firing processes ultimately led to a homogeneous, pore-free surface and excellent optical properties. MultiPlus titanium abutments were then bonded to the zirconium dioxide framework using dual-curing composite cement (PermaCem 2.0, DMG, Hamburg, Germany). Titanium posts were previously blocked out with wax and sandblasted with aluminum oxide. Sandblasting the titanium surface serves to obtain mechanical micro-retentions for an optimal bond between metal and composite cement.
Finishing and polishing of the cervical transition zones resulted in a high-quality joint-free framework- abutment connection. Since important clinical parameters like tooth length, tooth arrangement, esthetics, speech and chewing function had already been assessed at the time of the temporary restoration and transferred to the final prosthetic superstructure, prosthesis integration was predictable from a functional and esthetic point of view. However, should corrections be necessary, screw-retained detachable superstructure enable processing and corrections to be made extraorally effortless. A panoramic radiograph image obtained after bridge placement showed stable bone conditions and optimal fit.
Discussion: According to the currently valid S3 guideline “Implant-prosthetic care of the edentulous upper jaw” of the Working Group of Medical Professional Societies (AWMF) treatment with implant-supported restorations involves peri-implantitis/mucositis with a subsequent loss of osseointegration as well as loosening/fractures of the implant and denture components as possible biologicaland technical long-term complications (Schley et al. 2013). Conditionally removable prosthetic superstructures represent an ideal treatment option in case of such complications, since reconstruction detachment provides the clinician with good access to implants and simplifies extraoral repairs. The use of reduced number of implants, as in the present clinical case, corresponds to the knowledge currently available and reflects the current trend in implantology. According to the results of a current systematic review, high cumulative success rates could be determined when using four to six implants over an observation period of five years in both the upper and lower jaw (Mericske-Stern and Worni 2014). Even in patients presenting moderate and high bone resorption rates satisfactory long-term clinical results can be observed with partially removable, screw-retained prostheses on four to six implants splinted with bars in the edentulous upper jaw (Bueno-Samper et al. 2010). Further clinical studies showed that high success rates could be observed with screw-retained maxillary superstructures even on six unsplit implants after a mean observation period of eight years (Mertens and Steveling 2011). The loading protocol selection can be one of the decisive factors for the success of an implant-supported restoration, as a current systematic review has shown (Schimmel et al. 2014). Accordingly, failure rates for immediately loaded implants appear to be higher after the first year of loading than for delayed or conventional loading. For this reason, delayed loading of the implant-supported reconstruction appeared to be a more favorable solution than immediate loading. Chipping of the veneers is the most common complication in the case of full restorations made of zirconium dioxide framework and layered ceramic veneers (Heintze and Rousson 2010). In the present case, therefore, a CAD/CAM-milled monolithic zirconium dioxide bridge without layered ceramics was used.
Conclusion: The present case report shows that a restoration with six implants and a conditionally removable CAD/CAM bridge made of monolithic zirconium dioxide ceramic leads to functionally and esthetically pleasing clinical results. Only after a longer period of wear will it become clear to what extent the technical and biological complications described in the literature can be avoided with the chosen reconstruction. A simplified dental intervention is made possible in the event of complications. Transfer of functional and morphological parameters from the interim restoration to the design of the definitive reconstruction led to a predictable clinical outcome and high patient satisfaction.
Thanks: We would like to express our gratitude to MDT Nondas Vlachopoulos, Athens, for milling the Katana ML zirconium dioxide blanks.