Case report publication – Germany, 2021
Authors
Kleanthis Manolakis DDS Dr Med Dent
Pantelis Petrakakis, DDS Dr Med dent
Nikos Kournetas, DDS Dr Med Dent
Alexandros Manolakis DDS Dr Med Dent
Diamantis Tsifoutakos, MDT
Journal – Jahrbuch Implantologie 2021, Oemus Publishing Group
Introduction
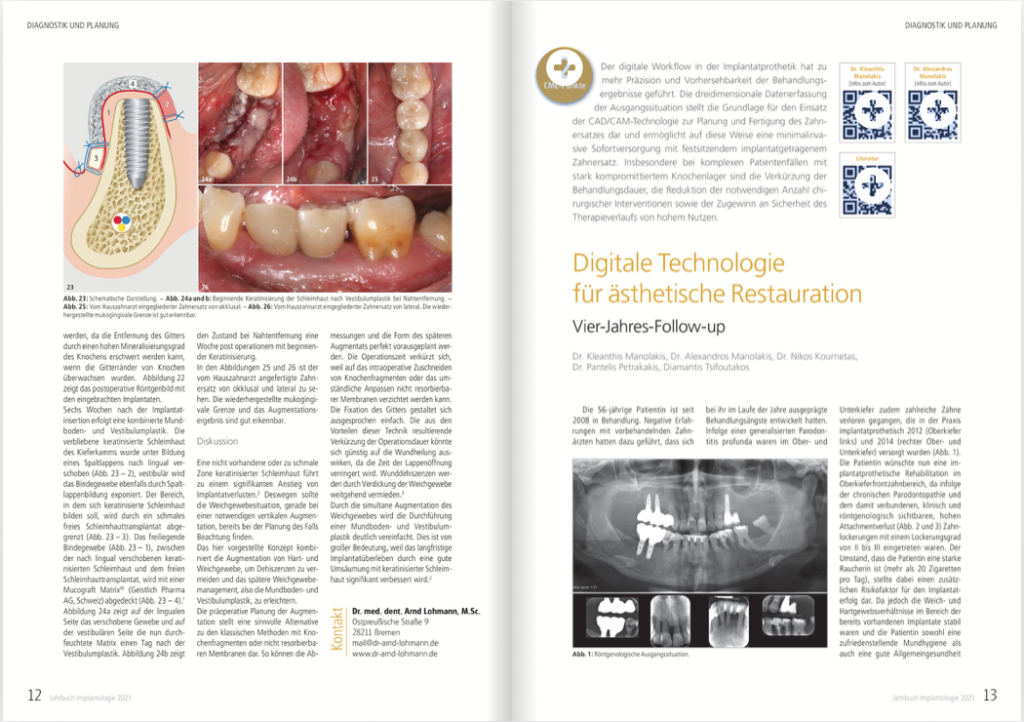
Digital workflow in implant surgery and prosthetics has led to additional precision and predictability of treatment outcomes. Three-dimensional initial situation data acquisition represents the foundation of use of CAD/CAM technology for the computer aided planning and computer aided manufacturing of provisional and final restorations. In this way a minimally invasive immediate restoration with fixed implant-supported restorations is enabled. Shortening of the treatment period, reduction of the necessary number of surgical interventions and increased safety are of great benefit, particularly in complex patient cases presenting severely compromised sites. The 56-year-old case presented in this case report has undergone treatment in our dental office since 2008. Negative experiences with dentists who had previously treated her had led to her developing fear of treatment over the years. As a result of generalized periodontitis profunda, numerous teeth had also been lost in the upper and lower jaw. There areas were restored in our practice with implant supported prostheses in 2012 (region of the left upper jaw) and in 2014 (region of the right upper and lower jaw). Patient now wanted implant prosthetic rehabilitation in the upper anterior region, as chronic periodontitis and associated clinically and radiologically visible extensive attachment loss had caused tooth loosening of degree II to III. The fact that the patient is a heavy smoker (more than 20 cigarettes per day) represented an additional risk factor for the success of the proposer treatment plan. However, since soft and hard tissue conditions in the existing implants areas were stable and she had both a satisfactory oral hygiene as well as good general health and a corresponding motivation for regular follow-up measures, implant therapy was carried out.
Diagnostics and treatment planning
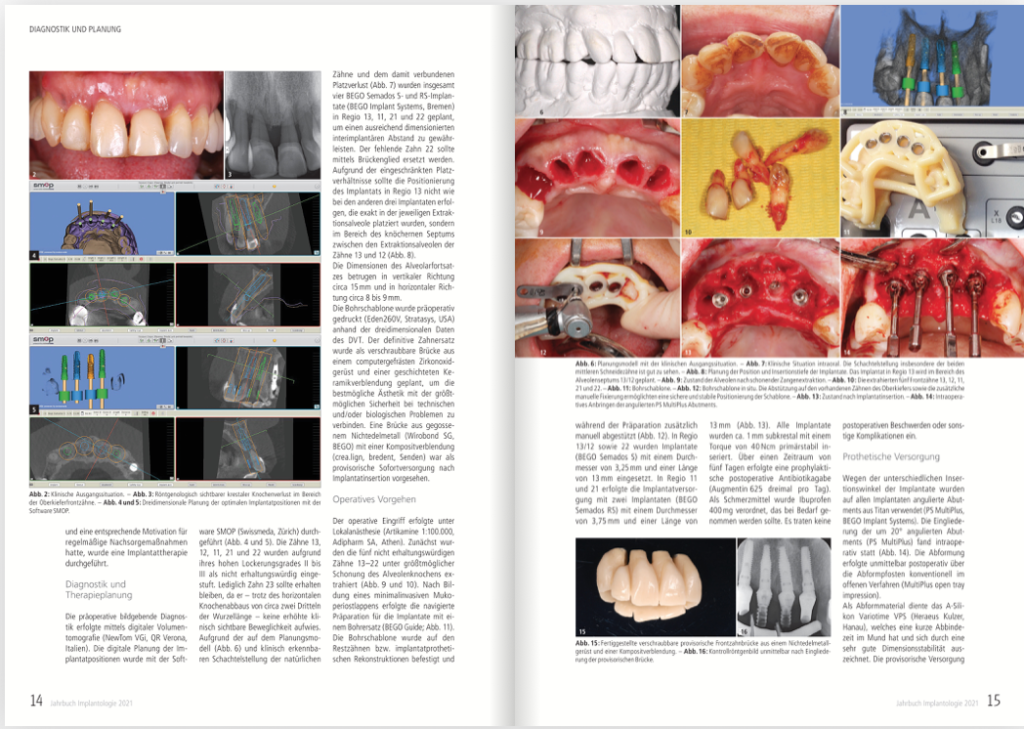
Preoperative diagnostic imaging was performed using digital volume tomography (NewTom VGi, QR Verona, Italy). Digital potential implant positions planning was carried out with SMOP software (Swissmeda, Zurich, Switzerland). Teeth 13, 12, 11, 21 and 22 were classified as not worth preserving due to their high loosening degree II to III. Only tooth #23 should be preserved; it did not present any clinically visible increased mobility, despite horizontal bone loss of about two thirds of the root length. A total of four Bego Semados S and RS implants (Bego Implant Systems, Bremen, Germany) were planned in regions 13, 11, 21 and 22 due to the nested position of the natural teeth and the associated loss of space to ensure adequately dimensioned inter-implant space. Missing #22 should be replaced with a pontic. Due to limited space available implant #13 should not be positioned like the other three implants, which were placed exactly in the respective extraction socket, but in the area of the bony septum between the extraction sockets of teeth #13 and #12. Crestal dimensions were approximately 15 mm in the vertical direction and approximately 8 to 9 mm in the horizontal direction. The drilling template was printed preoperatively (Eden260V, Stratasys, USA), based on three-dimensional CBCT data. The final restoration was planned as a screw-retained fixed partial denture made of a computer-milled zirconium oxide framework and veneered with layered ceramics. An additional FPD made of cast non-precious metal and veneered with composite (crea.lign, Bredent, Sending, Germany) was designed as a temporary immediate loading restoration at implant placement appointment.
Surgical implant placement
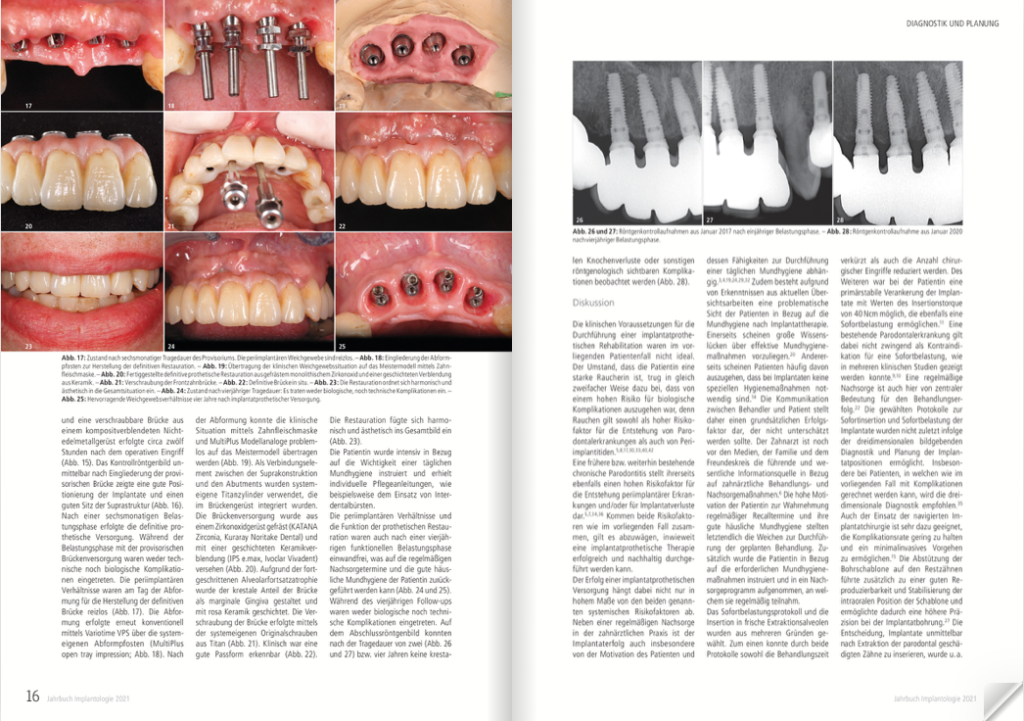
Surgical intervention was performed under local anesthesia (Artikamine 1:100,000, Adipharm SA, Athens, Greece). Initially five condemned teeth 13–22 were extracted while preserving the alveolar bone. After forming a minimally invasive mucoperiosteal flap, the navigated preparation for implant placement was carried out with a special set of drills for guided surgery. The drilling template was attached to the remaining teeth and implant supported reconstructions and additionally supported manually during the osteotomy. Titanium Bego Semados S implants of 3.25 mm diameter and 13 mm length were placed in regions 13/12 and 22. Two Bego Semados RS implants implants of 3.75 mm diameter and 13 mm length were placed in areas 11 and 21. Implants were inserted approx. 1 mm subcrestally and achieved a primary stability value of 40 Ncm. Prophylactic postoperative antibiotics (Augmentin 625 three times a day) were administered for a period of five days. There were no postoperative complaints or other complications observed.
Restorative treatment sequence
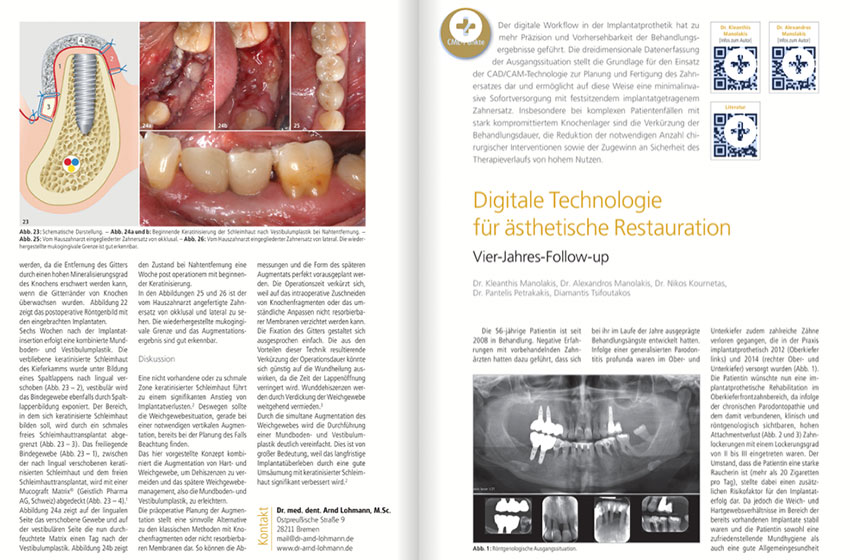
Due to the pre-planned angulated implant insertion, MultiPlus angulated titanium abutments were used. These 20° angulated abutments were integrated intraoperatively, in a one-abutment-one-time fashion. An impression was taken immediately postoperatively including the specially designed open tray multiunit impression posts using a conventional impression procedure. A-silicone Variotime VPS was used in this case (Heraeus Kulzer, Hanau, Germany), which displays short intraoral setting times and is characterized by optimal dimensional stability. The provisional screw-retained non-precious metal framework composite veneered restoration was placed approximately twelve hours following the surgical intervention. A control X-ray immediately after the provisional bridge showed that implants were well positioned and superstructure was well seated. Following a six-month loading phase the definitive prosthetic restoration took place. Neither technical nor biological complications occurred during the provisional loading phase.
Discussion
Clinical conditions for carrying out implant supported prosthetic rehabilitations were not ideal in the patient case presented. The fact that she is a heavy smoker contributed in two ways to the assumption that there was a high risk of biological complications. Smoking is considered to be a high-risk factor for the development of periodontal diseases and peri-implantitis. Previous or ongoing chronic periodontitis also represents a high-risk factor for the development of peri-implant diseases and/or implant loss. If both risk factors come together, as in the present case, it is important to weigh up the extent to which implant prosthetic therapy can be carried out successfully and sustainably. Success of an implant supported prosthetic treatment depends not only to a large extent on the two systemic risk factors mentioned. In addition to regular follow-up care in the dental practice, long-term success of implant supported restorations also depend in particular on patient motivation and their ability to carry out effective daily oral hygiene. On the one hand, there seem to be major gaps in knowledge about effective oral hygiene measures. Patients often seem to assume that no special hygiene measures are necessary when treated with implants. Communication between practitioner and patient is therefore a fundamental success factor that should not be underestimated. The restorative dentist is the leading and most important source of information regarding dental treatment and aftercare, ahead of the media, family and friends. The patient’s high level of motivation to attend regular recall appointments and her good oral hygiene at home ultimately set the course for carrying out the planned treatment. In addition, she was instructed on the necessary oral hygiene measures and included in an aftercare program, in which she regularly participated. The executed implant insertion into fresh extraction sockets and immediate loading protocol in the case presented was the treatment of choice for several reasons. On the one hand, immediate implant insertion and loading significantly shortened the treatment time and reduced the number of surgical interventions. Furthermore, primary stable anchoring of the implants with insertion torque values of 40 Ncm was possible in this clinical case, thus enabling immediate loading. Existing periodontal disease is not necessarily a contraindication for immediate loading, as has been shown in several clinical studies. Regular follow-up care is also of central importance for treatment success.
The selected protocols for immediate implant insertion and immediate loading were made possible not least as a result of the three-dimensional imaging diagnostics and planning of anticipated implant positions. Three-dimensional diagnostics is particularly recommended for cases where complications can be expected, as in the present case. Use of navigated implant surgery is also very suitable for keeping the complication rate low and enabling a minimally invasive procedure. Supporting the drilling template on the remaining teeth also led to good reproducibility and stabilization of the intraoral template position, thereby enabling greater precision during osteotomy preparation. The clinical decision of implant insertion immediately after extraction of the periodontally damaged teeth was made additionally to reduce further undesired alveolar bone resorption. Alveolar bone remodeling after tooth extraction is an unavoidable physiological process, occurring as a result of specific tooth support tissue loss (Sharpey’s fibers, lamina dura). Alveolar bone loss is more pronounced in the horizontal than in the vertical direction. This resorption pattern would have led to further reduction in the already severely compromised available bony implant bed. Immediate implant placement can achieve satisfactory preservation of the jaw ridge, provided buccal walls can be preserved after extraction. In the present patient case the dental prosthesis was made partially removable, even if there is a great deal of ambiguity in the literature with regard to the clinical advantages and disadvantages of the type of prosthetic attachment to implants. With regard to clinical parameters such as crestal bone loss, probing depths or bleeding indices, no differences were found between the two types of attachment, as a systematic review at the first Osstem Advanced Dental Implant Research and Education Center Consensus Conference in 2017 in the Italian city of Avegno showed. In other systematic reviews, on the other hand, it is stated that screw-retained implant-supported restorations should obviously lead to fewer biological and technical complications. Cement-retained implant prosthetic solutions appear to result in lower crestal bone loss rates and higher implant success rates than screw-retained prosthetic superstructures. What is certain is that both types of attachment have their specific problems. In the case of screw-retained restorations, loosening of the prosthetic screw and thus retention loss as well as veneer fractures are obviously the most common complications observed. Screw retained implant-supported restorations enable regular professional implant hygienic aftercare, if necessary, so one can intervene early in case of technical and/or biological complications. Another implant prosthetic factor with some risk potential was the use of angled abutments. Their influence on biological and technical complications in implant prosthetic restorations is also currently unclear. While a systematic review found no impact on peri-implant bone loss or implant survival rates, a recent meta-analysis found that the use of angled implants resulted in significantly higher crestal bone loss rates than non-angled abutments. Information on technical complications was not possible in either the systematic review or the meta-analysis due to limited data, according to the authors. In addition, no information was given on the extent of abutment angulation and its influence on complications. In the systematic review implant angulations between 15 and 30° were examined. In the present patient case, 20° angulation abutments were used. However, no complications occurred during the four-year follow-up period.
Summary
The present case report shows that even in suboptimal clinical conditions it is possible to provide long-term stable implant supported prosthetics. Using three-dimensional planning and navigated implant surgery even complex cases can be treated predictably and efficiently; without causing great stress to the patient in an immediate insertion and immediate loading protocol. In addition to the use of digital workflow, regular hygienic aftercare in the dental practice and regular oral hygiene at home is a major prerequisite for implant supported restorative long-term success.